Envisioning an End to FGM/C

Female genital mutilation or cutting—in which all or part of a girl’s or woman’s genitalia is altered or removed for nonmedical purposes—has been a traditional practice in many countries for over a millennium. More than 200 million women and girls alive today are FGM/C survivors.
In 2012, the UN General Assembly designated February 6 the International Day of Zero Tolerance for Female Genital Mutilation. Guided by Sustainable Development Goal 5, the UN aims for the elimination of the practice by 2030.
In this Q&A, adapted from the February 5 episode of Public Health On Call, Michele Decker, ScD, MPH, Bloomberg Professor of American Health in Population, Family and Reproductive Health, and Nicole Warren, PhD, MPH ’99, MSN, associate professor in the Johns Hopkins University School of Nursing, explain the importance of challenging long-standing cultural norms to end FGM/C, and the need to provide appropriate care for those who have experienced the practice.
They also discuss the launch of Johns Hopkins Center for Global Women’s Health and Gender Equity and some of its priority areas, including eliminating FGM/C.
Tell me about the Center for Global Women’s Health and Gender Equity. How did it come about, and why?
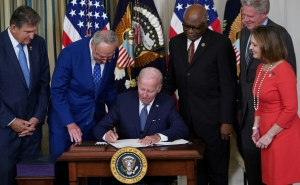
Michele Decker: We’re in a watershed moment for global women’s health and women’s rights. We see that in the Sustainable Development Goals. We see it in the inaugural U.S. National Plan to End Gender-Based Violence, the White House Gender Policy Council, and a number of other domestic and global policy initiatives that are elevating gender equity and women’s health.
The Center formed in October 2023 with the mission to advance global women’s health and gender equity through a combination of action-oriented research, training, and translation. We have an incredible wealth of gender equity and global women’s health research underway at Johns Hopkins. This new center allows us to synergize that expertise.
A couple of our priority areas are around eliminating gender-based violence and other harmful practices, including child marriage and female genital mutilation, as well as empowering women and girls and strengthening health systems to optimize gender equity.
Is this an international center? Or does it also have domestic components?
MD: We’ve got people working around the world, including in the U.S. We have gender equity issues right here in our backyard, like the gender wage pay gap and differential jobs and opportunities based on gender. And gender-based violence continues to be a leading driver of women’s morbidity and mortality, and it’s taking way too many people. We also have some U.S.-based work on FGM, or female genital mutilation or cutting.
We’re ready with the evidence base, and we’re ready for evidence-informed change.
Nicole, as an expert on FGM, can you tell us a little about that practice?
Nicole Warren: FGM is the acronym for “female genital mutilation.” That is the term the WHO and many other agencies use. It is a traditional practice that does not have any medical advantages, and that essentially harms some part of the female genitalia.
Is there a difference between FGM and FGC?
NW: As a nurse midwife, I tend to use the term “female genital cutting” because I want to use language that will be acceptable to my clients. Some people I care for absolutely do feel mutilated, and I use that term, FGM, if that’s what they’re using. Otherwise, I tend to use the term FGC, because I try to avoid creating that victim-perpetrator dynamic that just isn’t consistent with how some affected communities view the result of the procedure.
What is the traditional rationale for FGM/C?
NW: Communities would have many different answers, a lot of the rationales boil down to control—controlling behavior, minimizing the potential for promiscuity, and keeping people modest. It’s really about diminishing the potential for a girl or a woman to behave inappropriately. For many communities, FGC is also a way to ensure that she will be marriageable. And in some communities, marriage is what allows survival. So the impetus for families to continue the practice is really powerful.
I want to be clear that FGM/C is not required by any religion. In many countries, you see people of all faiths who practice FGC—Christians, Muslims, and those who follow traditional religions. It crosses financial, religious, and socio-cultural boundaries. Ministers of health do it just as folks who would be considered disenfranchised and poor.
Is this something that can be prevented through behavior change work?
MD: Absolutely—but not just at the individual level. These controlling norms have disproportionate and gendered harm, and we need to address those at the community normative level. We won’t get to prevention at the individual level alone.
NW: It’s really hard for an individual in a community to decide not to participate in the practice because social acceptability is a big driver. The sense of, “this is how female external anatomy looks most beautiful, looks most proper” means there’s a lot of demand for it from men and women.
There are also a lot of people who want to see the practice end, but right now, they’re still getting the cutting done because that risk-benefit ratio hasn’t quite tilted far enough. It is happening, but much more slowly than we’d like to see.
Could laws against FGM/C help?
NW: Well, some countries have laws and some don’t. Even in many countries where it’s illegal, there’s no enforcement. I have worked in Mali for quite some time, and they do not have a law on the books because there is a fear that it will drive the practice underground and make an unsafe practice even more unsafe.
MD: The limitations of criminalizing a behavior like this are a common thread across all forms of gender-based violence. It’s really important to have laws on the books, but it’s not a potent deterrent. We’ve got to think about the normative environment and address those social norms. We can’t just criminalize our way out of it.
You mentioned earlier that there’s a U.S. component to this.
NW: Where the U.S. gets involved is when women migrate here from countries where FGM/C is normative.
After people are affected by the practice, there’s a whole range of sequelae—medical, psychological, sexual, the list goes on. When people migrate to a place where FGC is not normative, they face health care systems and providers that don’t understand how their body is different and sometimes don’t even know the therapies available to treat those sequelae.
In the U.S., we have over half a million women and girls who are potentially affected by this practice, yet we have no consistent training for health care providers on the topic. We see higher C-section rates, for example, and other indicators of poor outcomes, and we can solve that. We can reduce the risks people face after they’ve been cut.
And when we can reduce that risk, develop a good rapport, and provide good care, now we hopefully have a trusting relationship to start talking about prevention. We can start talking about, “What are your plans for your daughter after you have this baby?” We can start thinking about making sure that primary prevention—preventing the first cut—also happens in the U.S.
Stephanie Desmon is the co-host of the Public Health On Call podcast. She is the director of public relations and communications for the Johns Hopkins Center for Communication Programs, the largest center at the Johns Hopkins Bloomberg School of Public Health.