Developing a National Strategy for Serosurveys in the United States
A Q&A with the authors of the report
There are now millions of confirmed cases of COVID-19 and the death toll has passed 100,000 in the U.S. Estimating the prevalence of infection and recovery is important for decision makers and public health workers at national, state, and local levels.
Serosurveys, which collect serology/antibody test data, could help map disease prevalence, showing both “hot spots” and areas where community transmission may have abated.
To help get the most value from serosurveys, the Center for Health Security has released a report, Developing a National Strategy for Serosurveys in the United States.
Gigi Gronvall, PhD, lead author of the report, breaks down some of the key points in this Q&A.
Who is this report intended for?
The report is intended for U.S. policymakers to help them make changes so that we can get the data needed for public health from antibody testing.
Lots of individual states and employers are initiating antibody studies called “serosurveys”, but without leadership to coordinate them, we won’t get as much value from this data. This hurts us now, because we won’t know the accurate prevalence of disease, and later, as we deal with the aftershocks years into the future.
Our report also provides a lot of background for anyone interested in what these serosurveys are, why they are done, and how to conduct them so that they provide the most useful information.
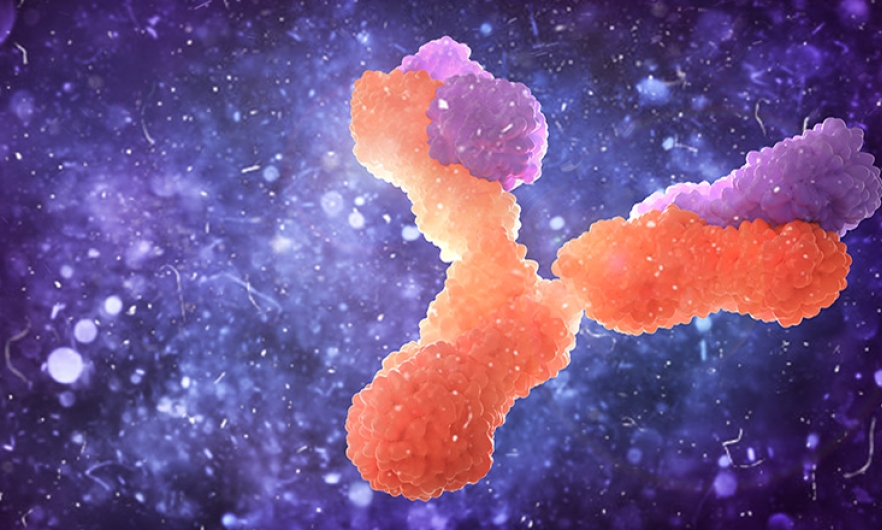
What is serology testing?
Serological tests, or “antibody tests”, detect evidence of the body’s immune response to an infection. These tests can provide information on prior infection with SARS-CoV-2, even after the immune system has successfully cleared the virus from the body.
Larger studies using antibody tests—“serosurveys”—can help us learn what proportion of the population has antibodies to the SARS-CoV-2 virus at a particular point in time and thus have been previously infected, even if they did not have symptoms or receive a diagnosis of COVID-19.
How can serology testing be a helpful tool?
Serology testing is important to understand the prevalence of SARS-CoV-2 infection.
It gives public health leaders situational awareness, so that sound decisions can be made about allocation of personal protective equipment (PPE), mitigation efforts, and, ultimately, vaccine procurement and prioritization when a vaccine becomes available.
Serology testing can be used to assess the effectiveness of various public health interventions to limit virus spread and determine the true case fatality rate of SARS-CoV-2 infections.
Long-term questions regarding medical sequelae can also be addressed—we don’t know yet if COVID-19 disease will have lasting effects on those who have had it.
What do serology tests NOT do?
Many people are interested in serology testing because they want to use it for individual decision making. They want to know if they have already had COVID-19 so they can be released from physical distancing measures.
This is, unfortunately, premature for many reasons. It does not appear that reinfections by SARS-CoV-2 are occurring, so for now, it appears that people who have had SARS-CoV-2 infection are protected. However, we don’t know how long that protection will last, and we don’t know whether or what levels of antibodies are important for protection.
In addition, many of the tests on the market right now are not very accurate. Because the prevalence of disease is relatively low, the impact of false positive results is magnified. At this time, antibody testing gives more information about a population than for an individual.
Are other countries using serology testing?
Many countries—including Spain, UK, China, Sweden, Germany, Netherlands, and Iceland—and U.S. states are using serology testing to make decisions about the effectiveness of public health measures and when and whether to “open up.” Large employers are using them, too. One of our recommendations is for the U.S. to provide a repository for all these studies like clinicaltrials.gov so that the information about all these studies can be in one place and useful to all.
What are “immunity certificates” and how might they be helpful or harmful?
Early on, several countries—including the U.S.—explored the idea that people who had already had COVID-19 could get a certificate releasing them from physical distancing measures and allowing them to go back to work. The idea was that the already immune could restart the economy.
Unfortunately, this idea is not workable for several reasons. For one, seroprevalence of SARS-CoV-2 infections is now quite low, so if only COVID-19-positive people were allowed to work, almost everyone would be excluded.
Second, there are scientific uncertainties about how long immunity will last, which would make issuing a certificate confusing.
Third, testing could be inaccurate because of flawed tests which has significant consequences. A false negative would keep a person from working, but a false positive could lead a vulnerable person to be exposed to SARS-CoV-2, possibly endangering themselves and others.
Fourth, requiring immunity for employment could create perverse incentives. Some people might try to get COVID-19 disease in order to be employed.
Finally, it would be difficult to roll out the distribution of immunity certificates in an equitable and unbiased manner given existing blindspots within vulnerable or minority communities.
Instead of immunity certificates, antibody tests need to be part of a suite of public health measures that may be used to decrease risks, along with masks, physical distancing, teleworking, etc. until a vaccine or other broad medical intervention can be available.
What are the key recommendations in the report? What actions should be taken and by whom?
Our report has four recommendations for how U.S. government agencies can provide leadership on antibody testing to get the most information out of the studies to promote shared learning and to prevent fraud and discrimination.
- The FDA should make the quality and accuracy of antibody tests clear to purchasers, because this affects the results of their use. Right now, many of these tests are being independently validated by U.S. agencies (like the National Cancer Institute), and the tests have been found to be significantly less accurate than the manufacturer claimed. The independent validation study results should be public and prominent.
- The CDC should coordinate serosurveys across states and public health departments, and develop a common protocol for states to use. All jurisdictions are facing similar challenges with trying to inform policy and mitigation strategies for COVID-19. National coordination of this effort would better utilize resources, improve efficiency and foster data harmonization, and decrease costs. Right now, states are designing and initiating their own studies, but the value would be greater if they had a shared protocol so results could be compared and so steps may be followed that give the study more statistical power and meaning.
- The U.S. government should create a central repository for serosurveys, similar to the function that ClinicalTrials.gov has for clinical trials. Given the demand for serosurveys for SARS-CoV-2 infection, sharing of information—including methodologies—is important. Such a repository could also be an international resource and could provide connections for others interested in initiating their own, similar studies. The CDC or another HHS agency could host such a site.
- The CDC should develop guidance for large employers/universities using antibody tests—which should include how such studies should and should not be interpreted—AND strongly encouraged these entities to register their studies in the central repository. There is potential for the results to inappropriately inform decision making by and about individuals, and the FDA and CDC state that serology tests should not be used to inform reopening of schools and businesses. Also, we don’t know what could happen in the years ahead. People who have had COVID-19 may develop other medical problems, and employers may use evidence of past infection in a discriminatory manner. Additional protective measures may need to be taken if discrimination based on SARS-CoV-2-specific antibody status occurs, but the first step is to have transparency that these tests are being used.