Johns Hopkins-Led Study Finds Convalescent Plasma Can Be Effective Early COVID-19 Therapy
Peer-reviewed publication in New England Journal of Medicine validates findings first announced in December

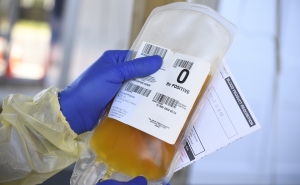
The New England Journal of Medicine (NEJM) today published final results of a nationwide multicenter study led by researchers at Johns Hopkins Medicine and the Johns Hopkins Bloomberg School of Public Health that show plasma from patients who have recovered from COVID-19 and whose blood contains antibodies against SARS-CoV-2, the causative virus, is an effective and safe option as an early outpatient treatment for the disease.
The research showed that high-titer (antibody-rich) COVID convalescent plasma—when administered to COVID-19 outpatients within nine days after testing positive—reduced the need for hospitalization for more than half of the study’s predominantly unvaccinated outpatients. The U.S. Food and Drug Administration currently authorizes this plasma as a treatment option for outpatients with immunocompromising diseases or receiving immunocompromising medications, and for all patients hospitalized with early-stage COVID-19.
The findings were first presented in a preprint posted to MedRxiv on Dec. 21, 2021. Details of the study, including authors and funding sources, may be found in the Johns Hopkins news release issued at that time.
“Based on our findings and conclusions—which are now validated through the peer-review process—we encourage health care professionals to keep SARS-CoV-2 antibody-rich blood plasma available in their blood banks as part of the treatment arsenal against early-stage COVID-19,” says study co-lead author David Sullivan, MD, professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health with a joint appointment in infectious diseases at the Johns Hopkins University School of Medicine.
“We believe that the best role for convalescent plasma is extending its use to early outpatient treatment when other therapies, such as monoclonal antibodies or drugs, are either not readily available—as in low- and middle-income countries—or ineffective, as with SARS-CoV-2 variants that are resistant to certain monoclonal antibodies,” Sullivan adds.
In the outpatient early-treatment study conducted between June 2020 and October 2021, the researchers provided 1,181 randomized patients with one dose each of either polyclonal high-titer convalescent plasma (containing a concentrated mixture of antibodies specific to SARS-CoV-2) or placebo control plasma (with no SARS-CoV-2 antibodies). The patients were 18 and older, and had tested positive for SARS-CoV-2 within eight days prior to transfusion. A successful therapy was defined as a patient not requiring hospitalization within 28 days after plasma transfusion.
The study found that 17 patients out of 592 (2.9%) who received the convalescent plasma required hospitalization within 28 days of their transfusion, compared with 37 out of 589 (6.3%) who received placebo control plasma. This translated to a relative risk reduction for hospitalization of 54%.
Timing of the convalescent plasma transfusion also is critical: “The earlier the better,” the researchers say.
“Based on the findings of an analysis in the new paper that wasn’t available when the preprint was posted, we found that if convalescent plasma is given within five days after diagnosis, the effectiveness at reducing hospitalization approximated 80%,” says Sullivan.
“We concluded that these results strongly support high-titer SARS-CoV-2 convalescent plasma as an effective early treatment for COVID-19 with advantages such as low cost, wide availability and rapid resilience to the virus’s evolving variants,” says study co-lead author Kelly Gebo, MD, MPH, professor of medicine at the Johns Hopkins University School of Medicine.
The next step, the researchers say, is to make convalescent plasma for the outpatient treatment of COVID-19 easier to use, more efficiently administered and more accessible to those who might need it. As part of that effort, they have provided clinicians with a guide for implementing a plasma transfusion center for outpatients with COVID-19, including logistical, staffing and blood banking requirements. The guide appears in a paper published March 29, 2022, in the journal Transfusion.
The team also continues to seek more understanding of what else convalescent plasma can do for outpatients with COVID-19. A soon-to-be published study will look at the ability of plasma to neutralize SARS-CoV-2 variants, including delta and omicron, despite no previous donor exposure to those viruses.
Since the study findings were first announced last December, there have been three developments supporting the use of convalescent plasma for early-stage COVID-19:
- On Dec. 28, 2021, the FDA expanded the authorized emergency use of convalescent plasma with high titers of anti-SARS-CoV-2 antibodies “for the treatment of COVID-19 in patients with immunosuppressive disease or receiving immunosuppressive treatment, in either the outpatient or inpatient setting.”
- On Feb. 2, 2022, the Infectious Disease Society of America updated its “Guidelines on the Treatment and Management of Patients with COVID-19” to include the “use of convalescent plasma in ambulatory patients with mild-to-moderate COVID-19 at high risk for progression to severe disease with no other treatment options.”
- On March 7, 2022, the American Red Cross announced that it was “temporarily testing all blood donations for COVID-19 antibodies to help identify donations that could be processed into convalescent plasma.” The organization said this was being done “to help support immunocompromised patients battling COVID-19.”
“These recent acknowledgements of high-titer convalescent plasma’s benefit in treating early-stage COVID-19—in conjunction with our peer-reviewed findings and our new guide for more effective administration of the treatment—provide clinicians with an additional option for outpatients,” Gebo says.
# # #
Media contacts: Barbara Benham at bbenham1@jhu.edu and Michael E. Newman at mnewma25@jhmi.edu.
Note: This news release was also published in the Johns Hopkins Medicine Newsroom.