Clinical Research and Epidemiology in Diabetes and Endocrinology
Leadership

Todd T. Brown, MD, PhD
PROGRAM DIRECTOR
Professor of Medicine and Epidemiology
Division of Endocrinology, Diabetes, and Metabolism

Sheela N. Magge, MD, MSCE
PROGRAM DIRECTOR
Professor of Pediatrics
Director, Division of Pediatric Endocrinology and Diabetes

Wendy L. Bennett, MD, MPH
PROGRAM DIRECTOR
Associate Professor of Medicine
Research Director, General Internal Medicine
Overview
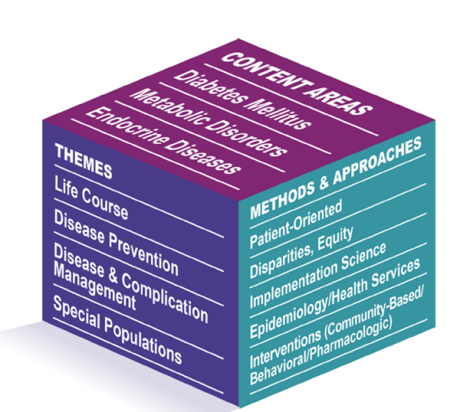
An integrated matrix of content areas, themes, and methods facilitates training, mentoring, and research success.
Diabetes mellitus has reached epidemic proportions in the US and abroad. Other endocrinologic diseases, like hypothyroidism and osteoporosis are also extraordinarily common. Patient- and population-oriented researchers with expertise in these conditions are urgently required. With this need in mind, in 2002, we established a training program at Johns Hopkins devoted to clinical and epidemiologic research in diabetes and endocrinology and funded by the National Institute of Diabetes, Digestive, and Kidney Diseases (NIDDK). More than 20 years later, it remains the only one of its kind in the US. The training program appoints two pre-doctoral students and three post-doctoral fellows per year and leads them to the MHS or PhD in clinical epidemiology, clinical investigation, or related field. Thus far, we have successfully trained over 50 young scholars who have produced scores of peer-reviewed scientific papers and who hold research positions across the country.
Our approach to training recognizes that the major discovery opportunities of this era are most effectively harnessed by individuals who embrace the interfaces between disciplines. Consistent with this, our training program is based on a multi-dimensional matrix structure, which integrates our expertise in the investigation of diabetes and endocrine diseases, cross-cutting themes, and use of core resources, investigative methods, and analytical approaches to maximize opportunities for success amongst trainees.
Further, this framework allows us to actively draw on the collective expertise of our faculty. Using this model, trainees are given access to state-of-the-science methods and approaches supported by multi-layered individualized mentoring teams. We will teach trainees how to harness the power of synergistic investigative teams to conduct optimal translational science. The model assists with conceptualizing individual research projects, helping to identify potential synergies and to connect trainees with an appropriate mentoring team for their current project and for their longer-term career development.
Program Strengths
The strengths of this program include:
- Strong existing diabetes and endocrine research collaborations between the Division of Endocrinology, Diabetes and Metabolism; Division of Pediatric Endocrinology; the Welch Center for Prevention, Epidemiology, and Clinical Research (Welch Center); the School of Public Health; and the School of Nursing
- Outstanding thesis-based degree programs in Epidemiology and Clinical Investigation at the School of Public Health
- Outstanding clinical expertise in diabetes and endocrine disorders
- Seasoned mentors experienced in grooming young scientists for academic careers, and
- High-caliber trainees wanting to pursue clinical and epidemiologic research careers related to diabetes and other endocrinology disorders.
Program Features
Program Options
Our pre-doctoral fellows are eligible for tuition support for their PhD program. Our post-doctoral trainees have the opportunity of pursuing a MHS or PhD in the Graduate Training Program in Clinical Investigation.
Faculty Mentors
Affiliated Research Centers and Departments
Division of Endocrinology, Diabetes, and Metabolism
The Johns Hopkins Division of Endocrinology, Diabetes, and Metabolism offers expert care for various metabolic, pituitary, thyroid and diabetes-related conditions. Our team is committed to delivering compassionate care, advancing novel research and educating the next generation of health experts.
Division of Pediatric Endocrinology and Diabetes
The Division of Pediatric Endocrinology and Diabetes offers a wide variety of clinical services, research and training opportunities. In addition to the diagnosis and treatment of endocrinological problems, our faculty members are also involved in a variety of basic science and clinical research.
Division of General Internal Medicine
The Johns Hopkins Division of General Internal Medicine is home to a large, diverse group of individuals dedicated to our mission to provide the best care to patients and populations, educate and mentor the next generation of physicians and scientists, and improve health and healthcare through innovative research.
Welch Center for Prevention, Epidemiology and Clinical Research
The Welch Center is where interdisciplinary faculty and trainees collaborate on groundbreaking epidemiologic, clinical, and translational research related to preventing and controlling chronic diseases.
Bloomberg School of Public Health's Department of Epidemiology
The Johns Hopkins Bloomberg School of Public Health's Department of Epidemiology improves the public’s health by training epidemiologists and advancing knowledge concerning the causes and prevention of disease and the promotion of health.
Johns Hopkins School of Nursing
Whether you are a new graduate, a seasoned and experienced nurse, or are simply seeking a new direction, Johns Hopkins Nursing has a role for you.
Johns Hopkins Center for Health Equity
The Johns Hopkins Center for Health Equity works to make healthcare institutions more equitable, communities more engaged, and health policies and practices more effective to eliminate disparities in health and healthcare in Baltimore, the United States, and the world.
Center for Human Nutrition
Applying the lens of justice and equity, the Center for Human Nutrition tests and implements nutritional policies and interventions to enhance dietary and nutritional well-being and health of populations, with an emphasis on women, children, and adolescents in underserved populations worldwide.
Johns Hopkins Center for Women's Health, Sex, and Gender Research
The Johns Hopkins Center for Women's Health, Sex, and Gender Research is a collaboration among the Bloomberg School of Public Health, the Johns Hopkins School of Medicine, and the Johns Hopkins School of Nursing. Together we promote collaborative research on women’s health and gender differences in health.
Baltimore Metropolitan Diabetes Regional Partnership
Learn more about the Johns Hopkins Medicine Diabetes Prevention and Education Program (DPEP) — home to the Centers for Disease Control and Prevention’s (CDC) National Diabetes Prevention Program (DPP) and the American Diabetes Association-recognized Diabetes Self-Management Training (DSMT) programs.
For additional information about the training program, contact:
Todd T. Brown, MD, PhD
Director, T32 Clinical Research and Epidemiology
in Diabetes and Endocrinology Training Program
Email: tbrown27@jhmi.edu
