Highlights of the Digital Healthcare Equity Framework
Issue 16, October 2024
The Digital Healthcare Equity Framework and its Implementation Guide are designed to ensure that digital healthcare solutions are developed and applied in ways that reduce, and not exacerbate, healthcare disparities. Created by our guest editors, Dr. Elham Hatef and Dr. Matt Austin, as part of a contract through the U.S. Agency for Healthcare Research and Quality, these resources offer foundational guidance that can be applicable to many types of settings. However, as highlighted below, global digital health practitioners will need to adapt certain recommendations for low-resource settings and ensure that their use of the framework is tailored to the specific contexts in which they operate. Ultimately, advancing health equity through digitization requires access to high-quality healthcare for all people, including historically marginalized groups, in a manner that reduces, rather than exacerbates, existing disparities and harms.
Guest Editor's Remarks:
The advancement of digital healthcare technologies has resulted in many viable solutions that can improve healthcare delivery and outcomes. However, all too often, any phase of a digital healthcare solution can fail to consider the unique needs, capabilities, and characteristics of all patient groups, leading to healthcare inequities when implemented. We created a Digital Healthcare Equity Framework (the Framework)—an evidence and consensus-based framework that guides users in intentionally considering equity in healthcare solutions that involve digital technologies. We also wrote an accompanying Implementation Guide (the Guide) to assist digital healthcare stakeholders—solutions developers and vendors, healthcare systems, providers, and payers—with developing and using digital healthcare technologies that are equitable so they do not create new or exacerbate inequities and disparities.
To create the Framework and Guide, our team conducted an environmental scan and key informant interviews on the existing, related frameworks and best practices, reviewing both domestic and international sources. Next, a 31-person technical expert panel was convened to discuss perspectives on digital healthcare and health equity, and ultimately to inform the development of the Framework and the Guide.
The Framework serves as a tool to help users and other stakeholders assess whether healthcare solutions involving digital technologies are equitable at every phase of the digital healthcare lifecycle. The Guide contains best practice examples and relevant resources to help users implement the Framework. The Framework and the Guide apply to both patient-facing and clinician-facing healthcare solutions, addressing the accessibility, purpose, security and privacy, usability, and safety concerns of those digital solutions.
Overview of the Digital Healthcare Equity Framework:
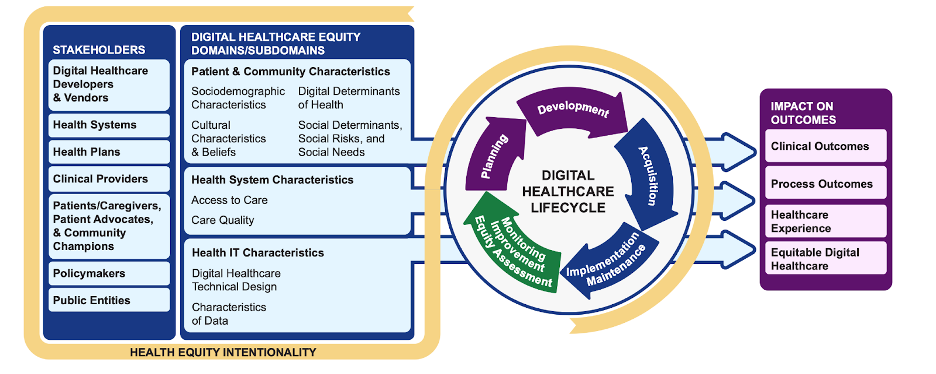
- Aims to improve clinical outcomes, healthcare processes, and patient experiences. It also seeks to achieve equitable access to, and equity in, the quality of healthcare solutions involving digital technologies.
- Designed for use by all stakeholders who are critical in ensuring that healthcare solutions promote equity, namely digital healthcare solutions developers and vendors, health systems, health plans, and clinical providers.
- Organized and structured around the digital healthcare lifecycle, consisting of five structured phases that intentionally incorporate an equity assessment in each one: Planning, Development, Acquisition, Implementation/Maintenance, and Monitoring/Improvement/Equity Assessment.
- Considers factors from three main domains:
- Patient and Community Characteristics: socio-demographic details, cultural beliefs, digital determinants, and social risks.
- Health System Characteristics: access to care, care quality, and affordability.
- Health Information Technology Characteristics: technical design of digital solutions and the accuracy, transparency, and ethical handling of data used and generated.
Key Implementation Recommendations and Considerations for Low-Resource Settings:
Overview of the Implementation Guide:
- Organized according to the digital healthcare lifecycle phases and the primary stakeholders implicated for these phases.
- Provides actionable recommendations for each phase of the digital healthcare lifecycle, with illustrative real-world examples for each.
- Suggests how to engage other stakeholders who are not the primary ones for that phase.
Implementation Phase Recommendations and Tips for Low-Resource Settings:
Planning and Development Phases
Key Stakeholders: Digital Healthcare Developers and Vendors
Purpose: To enhance access to care for underserved populations, software developers and vendors should engage marginalized communities, integrate cultural sensitivity, and ensure accessibility for users with disabilities.
Key Recommendations:
- Engage potential users of the technology, especially those from marginalized communities: Developers should actively involve potential users of the technology, especially those from historically marginalized groups, during this phase to ensure the digital healthcare solution meets their unique needs. For instance, during the COVID-19 vaccination rollout, tailored approaches helped target elderly populations in the U.S., addressing challenges related to accessibility.
- Understand cultural characteristics: Designing solutions that reflect the cultural beliefs and beliefs of the target population is essential for their success. Real-world examples, such as engaging black men to understand how racism influences their trust in the U.S. healthcare system, highlight the importance of cultural sensitivity in designing solutions that might require them to disclose sensitive information.
- Design the technology in a manner that helps–and does not hinder–access to high-quality care. Solutions developers need to anticipate potential barriers to healthcare access that the digital tool might create. Some strategies that have proven useful include:
- Ensure inclusivity for disabilities: Incorporate features such as voice-activated technology and accessible interfaces, in digital healthcare solutions
- Test for racial, ethnic, and gender bias: Rigorously test digital health tools, such as medical devices, on diverse populations to avoid biases. For example, pulse oximeters were found to be less accurate on darker-skinned patients, highlighting the importance of unbiased testing.
- Ensure equitable and transparent data use in solution design: To foster trust and accountability, digital healthcare solutions should apply policies and controls that protect patient data, including allowing patients to control data-sharing permissions. Moreover, when choosing data for training and testing their technologies, developers should use samples that are representative and inclusive of their user population as well as be transparent about which data models were used.
CGDHI Considerations for Low-Resource Settings:
In low-resource settings, engaging marginalized communities in the planning phase is crucial to address the digital divide and ensure that digital healthcare solutions meet their specific needs. Solutions must be adaptable offline to ensure functionality in rural or underserved regions. Moreover, developers must focus on scalable solutions that account for limited device ownership and internet access, while maintaining affordability to enhance inclusivity. The gender digital divide is also a significant consideration, making it essential to develop digital solutions that are fully accessible to women and girls. Incorporating account management functionality, privacy safeguards, and interoperability with existing systems is especially critical in contexts of limited device ownership, where device-sharing is common. Without personalized account management, privacy can easily be compromised when multiple users share the same device, which disproportionately affects women and youth who may have less control over devices. Additionally, interoperability ensures that digital health solutions can integrate with existing platforms, allowing users to access services seamlessly, even when sharing devices. Finally, it is important to remember that digital health equity can also be achieved through non-digital solutions such as a simple phone call for appointment scheduling.
Acquisition and Implementation/Maintenance Phases
Key Stakeholders: Health Systems, Health Plans, and Clinical Providers
Purpose: To provide accessible, high-quality care for all populations, recommended steps include adopting digital inclusion strategies, engaging in participatory collaboration, assessing the impact of digital solutions on equity, and ensuring technical compatibility.
Key Recommendations:
- Adopt digital inclusion strategies: Health systems and providers should implement digital inclusion strategies to reduce barriers and ensure equitable access to digital healthcare solutions. For example, the Affordable Connectivity Program helps U.S. households afford the necessary broadband for healthcare, work, and education.
- Encourage participatory collaboration: A multisectoral approach engaging various stakeholders is vital for successful acquisition and maintenance of digital solutions. During the COVID-19 pandemic, Pima County Health Department in Arizona collaborated with housing departments to address health disparities and deliver crucial vaccination information to underserved populations.
- Assess impact on equity across different types of health systems when implementing digital solutions: To avoid exacerbating disparities, healthcare solutions must be evaluated systematically on equity, especially regarding access and care quality before implementation.
- Ensure inclusivity of languages: Offering digital health platforms in multiple languages ensures that all patients can benefit from digital health technologies.
- Invest in community-based organizations and local partnerships: Community organizations may be available to assist in increasing access to digital healthcare solutions, by providing internet-enabled devices in underserved areas.
- Designate personnel as digital literacy navigators: Train health professionals in digital health literacy sensitivity to help patients access, navigate and use digital healthcare technologies, to ensure equitable access to quality care as well as continuity of care.
- Consider development and maintenance: Before acquiring a healthcare solution, it is essential for health systems to evaluate how it was developed, where and how it will be implemented and maintained, and how it will use, produce, or transmit data to ensure it aligns with equity goals.
CGDHI Considerations for Low-Resource Settings:
In the context of low-resource settings, we must consider infrastructural variability, where intermittent power and unreliable network coverage can significantly hinder the scalability of digital health solutions. Collaboration with local governments to subsidize essential digital infrastructure could enable long-term sustainability, while open-source platforms could drive down costs and encourage wider adoption. Furthermore, equipping community health workers or other frontline workers with mobile technologies can serve as a bridge to address gaps in digital literacy and technical expertise within the broader population. Addressing digital literacy through targeted training programs for providers and patients can help bridge gaps in understanding and utilization of such solutions, fostering long-term success in the adoption of digital healthcare tools.
Monitoring/Improvement/Equity Assessment Phase
Key Stakeholders: Health Systems, Health Plans, and Clinical Providers
Purpose: To ensure continuous and equitable improvements in digital healthcare solutions, recommended steps include engaging communities through participatory approaches, requiring health systems to identify excluded populations, and addressing communication and accessibility barriers.
Key Recommendations:
- Identify and address excluded populations: Health systems should assess which populations are using digital technologies and identify any groups that are excluded or not benefiting equally. For example, the California Department of Managed Health Care stratified data by race and ethnicity to understand equitable quality of healthcare delivery.
- Use a participatory approach: Actively engage affected community members to gather input on the barriers to the usage of digital healthcare solutions. To do so effectively and inclusively, account for the users’ communication preferences. Offer translation services, gather input through surveys, virtual focus groups or other appropriate methods, and provide accommodations for people with disabilities to ensure their voices are heard.
- Ensure digital solutions facilitate access: Continuously evaluate how the digital solution impacts access to quality care. Establishing long-term partnerships with community organizations for digital literacy training, collaborating with experts to identify underserved groups, and implementing applications that promote user self-sufficiency and engagement can help ensure that all community members benefit equally from new technologies.
- Address data gaps for continuous monitoring: Identifying and addressing data gaps is essential for comprehensive monitoring and equity assessments of digital health solutions. To do so, review data for patterns of missing data points and disaggregate data by key demographics such as race, gender, and socioeconomic status.
Comment from the Center for Global Digital Health Innovation on Considerations for Low-Resource Settings
Monitoring and improving digital healthcare equity in low-resource settings requires innovative approaches to data collection and community engagement. Identifying excluded populations can be challenging due to the lack of comprehensive data systems, making the integration of offline and low-tech solutions essential. For instance, community health workers can bridge digital gaps by manually gathering health data and providing services in areas with limited digital access. Moreover, participatory approaches should be adapted to local contexts, through the use of face-to-face consultations or SMS-based surveys in regions with low internet penetration. To ensure continuous improvement, local health systems need to develop low-cost, scalable methods to disaggregate and analyze data, particularly for two factors often overlooked in traditional health metrics: gender and socioeconomic status. This emphasis on offline and low-tech methodologies would create a more equitable digital health landscape, tailored to the realities of low-resource settings.
General Recommendations for Implementing Digital Healthcare Equity

Assess organizational readiness
Evaluate for key drivers of digital healthcare equity: leadership commitment, economic viability, health IT capabilities, and change management capacity.

Identify an equity champion
Designate a leader to drive sustainable, long-term equity initiatives across all digital healthcare development and implementation phases.

Hire a diverse workforce
Build a staff team with various lived experiences, helping ensure that organizational culture and projects prioritize digital healthcare equity.

Monitor progress towards digital healthcare equity
Foster continuous improvement through regular equity assessments, feedback loops, and the use of metrics and dashboards to track achievements.
Click the links below to read previous editions of Research Roundup and to receive the latest updates in global digital health!
Meet Our Guest EditorS
Dr. Elham Hatef is a board-certified, preventive medicine physician and clinical informatician. She is an associate professor in the Division of General Internal Medicine, Department of Medicine at Johns Hopkins School of Medicine, with a joint appointment in the Department of Health Policy and Management at Johns Hopkins Bloomberg School of Public Health. Her main field of interest is health disparities and the impact of social needs and social determinants of health on health-related outcomes using health IT and real-world data.
Dr. Matt Austin is a principal faculty member at the Johns Hopkins Armstrong Institute for Patient Safety and Quality in the School of Medicine. His research focuses on performance measurement in healthcare. His current research interests include understanding the role of transparency of quality and safety data in driving improvements in care delivery, measuring disparities in the quality of care, and measuring the diagnostic performance of hospitals. Matt earned his Ph.D. in industrial and systems engineering from the University of Wisconsin–Madison.
