Malaria’s Latest Foe? Bacteria.
A naturally occurring bacterium and a compound it secretes show potential for malaria control.
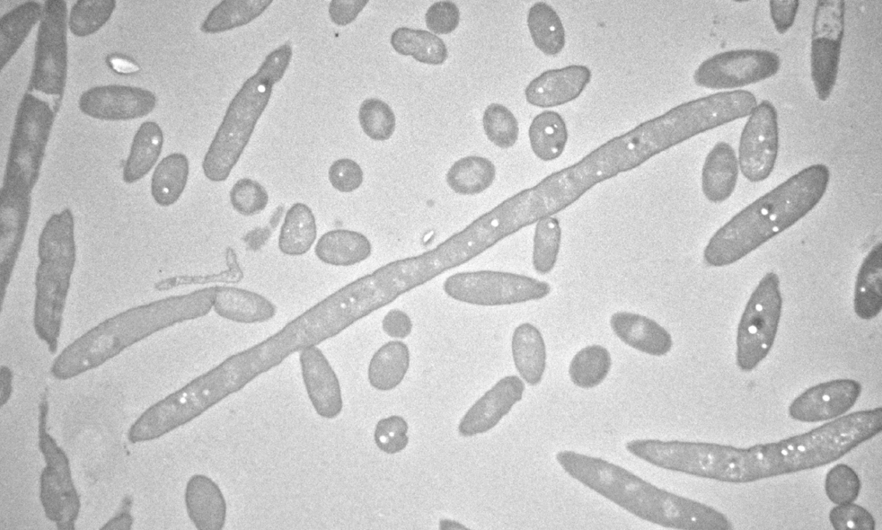
Transmission electron microscope image of Delftia tsuruhatensis. Photo: Isabelle Coppens
Over the past century, malaria control interventions have changed little. Insecticides remain the staples of prevention, but as mosquitoes and the malaria parasite continue to adapt and develop resistance, innovative, novel methods are needed.
In a new paper published in Science, Marcelo Jacobs-Lorena, PhD, professor emeritus in Molecular Microbiology and Immunology, and his colleagues, in collaboration with researchers at GSK Global Health Medicines R&D, show that a naturally occurring bacterium and a chemical it secretes inhibit the malaria parasite’s development in mosquitoes—meaning they can’t transmit the parasite to humans.
The method has distinct advantages: It’s low-tech, easily reproducible, and uses no genetic modification techniques. And, Jacobs-Lorena says, it can work in perfect concert with existing effective control strategies.
How did this project get started?
It began at GSK laboratories in Spain, where scientists were working on malaria drugs. To test those drugs, they had a colony of mosquitoes that they regularly infected with Plasmodium falciparum [the malaria parasite]. Over time, the researchers were not able to infect these mosquitoes anymore. They looked for possible causes and found that a strain of Delftia tsuruhatensis [which they named Tres Cantos 1, or TC1] was present in all screened mosquito samples.
Initial tests showed that if the mosquitoes carried TC1, the development of the parasite in the mosquito was compromised. To continue this line of research, they contacted me, asked to collaborate, and then they sent us the bacteria.
How exactly did you test this theory?
First, we fed the TC1 bacteria to the mosquitoes in our lab’s colony and confirmed that the bacteria inhibited development of the parasite in the mosquito. Next, a senior research associate in my laboratory, Wei Huang, discovered that if you culture the bacteria and then feed the mosquitoes with the supernatant [liquid from the culture excluding cells], parasite development was inhibited. That told us that the supernatant contains the inhibitor and that the bacteria act by secreting an inhibitor that attacks the parasite.
At this point GSK contracted Fundación MEDINA to fractionate [separate a mixture into its component parts] the supernatant to identify the inhibitor. They sent individual fractions back to us, and we tested them by feeding mosquitoes each fraction mixed with infected blood. In this way, we determined which fraction contained the inhibitor.
Ultimately scientists at Fundación MEDINA identified the compound as harmane. It turns out that harmane can easily be purchased from chemical companies. We ordered the compound and confirmed that the compound inhibits the parasite.
Then Wei had the idea of testing something different: he dried the harmane on a glass plate, let the mosquitoes sit on that plate for one hour, and then fed infected blood to the mosquitoes. He found that the mosquitoes that sat on harmane had strongly impaired development of the parasites, meaning harmane can penetrate the mosquito cuticle [outer part of the leg] and inhibit the development of the parasite.
How could these findings benefit malaria control measures?
I think it is important to put things in perspective. Up until now, a full century of efforts to control malaria were done by killing the mosquito using insecticides. The use of this bacterium to turn the mosquito into a “non-transmitter” is a new way to combat malaria. The other very important discovery that we made is that once the mosquito acquires the bacterium, it stays with the mosquito for the life of the mosquito.
How could this be implemented in the field?
Lots of research has been done in the field using sugar baits—a blend of sugar and mosquito attractants mixed with insecticide to kill the mosquitoes. The proposal here is, instead of mixing the sugar baits with an insecticide, to mix it with bacteria so the mosquitoes can feed on it. This method has the advantage that there are lots of experiments being done in the field using sugar baits, so the technology has been perfected already. Initial implementation experiments in Burkino Faso yielded promising results, demonstrating the potential of this intervention for malaria control.
Another possibility is to incorporate harmane into bed nets or spray it on walls.
How effective would using these bacteria be at reducing malaria deaths?
The modeling study described in the paper [done by Imperial College London] shows that if you combine this approach with distribution of long-lasting bed nets and other measures, a further 15% reduction in clinical cases of malaria can be achieved. In other words, many more lives would be saved.
But it’s good to make this point clear: By using this approach alone, you will not eliminate malaria. There is an absolute need to use a multi-pronged approach, including insecticides, vaccines, and drug treatment. We have to combine everything we have.
What excites you most about these findings?
What excites me most is the approaching reality of introducing a new strategy to combat malaria. If you do the calculation, one child dies every minute of malaria in Africa. The other thing is that this bacterium is not genetically modified. That is a big deal when you talk about implementation—translation from the laboratory to the field. There are laboratories developing genetically engineered mosquitoes that kill the parasite in combination with gene drive, a method to make those inhibitory genes spread through mosquito populations, and this has some promise. But you’re talking about releasing genetically modified organisms in nature, and this is a big barrier in terms of regulation and acceptance by local populations.
The fact that this is a naturally occurring bacterium that was originally isolated from a mosquito, and that Delftia tsuruhatensis is widespread in nature, excites me. This means that it can be tested out in the field in a much shorter term than other approaches that use genetic modification either of mosquitoes or of bacteria.
Morgan Coulson is an editorial specialist in the Office of External Affairs at the Johns Hopkins Bloomberg School of Public Health.





