Why Rotavirus Vaccine Introduction in Nigeria is a Milestone for Child Health

In August 2022, Nigeria became the most recent country to introduce the rotavirus vaccine into its national immunization program. The integration of the rotavirus vaccine into Nigeria’s routine immunization schedule is expected to help reduce at least 40% of morbidity and mortality associated with rotavirus infections amongst children.
Key Points
- Nigeria’s recent introduction of rotavirus vaccine into its immunization schedule has the potential to save the lives of nearly 100,000 children under five over the next decade.
- Immunization against rotavirus significantly reduces diarrhea-related hospitalizations and can relieve pressure on overburdened health systems.
- Rotavirus vaccines provide a return on investment and protect families from potentially catastrophic medical expenses.
- By preventing diarrheal disease and the malnutrition that may be associated with rotavirus infection, rotavirus vaccines can reduce the risk of stunting and promote healthy cognitive development.
Diarrheal diseases are one of the leading killers of children worldwide, claiming the lives of an estimated 484,000 children under five each year1. Though many bacteria and viruses can cause diarrhea, rotavirus may be responsible for up to 38% of diarrhea-related hospitalizations in children under five in countries where the rotavirus vaccine has not yet been introduced2. The burden of rotavirus is concentrated in low- and middle-income countries, with a 2013 study reporting that nearly half of all global rotavirus deaths occurred in just four countries: India, Nigeria, Pakistan, and Democratic Republic of Congo3. Because rotavirus is so highly transmissible, preventing rotavirus infection with the use of rotavirus vaccines is more effective than treating symptoms after infection.
In August 2022, Nigeria became the most recent country to introduce the rotavirus vaccine into its national immunization program. This measure will protect millions of vulnerable children and significantly lower the global burden of rotavirus disease. “Nigeria’s rotavirus vaccine introduction has been a long-awaited event, making the inaugural rollout a milestone moment for Nigeria as well as the rest of the world united in efforts to reduce the mortality and morbidity of diarrheal diseases caused by rotavirus,” wrote ROTA Council Chair Mathu Santosham. “The implications of this launch event are tremendous.”
Due to the country’s high disease burden, introduction of the vaccine in Nigeria has the potential to avert a significant number of rotavirus hospitalizations and deaths. The mortality rate for rotavirus in children under five in Nigeria is estimated to be 136 per 100,000, accounting for 30% of all global rotavirus deaths in children under five4. Introducing the rotavirus vaccine into Nigeria’s national immunization program has the potential to protect 6.9 million children from this disease each year5, and it could potentially save the lives of nearly 100,000 children over the next decade6.
Relieving Pressure on Health Systems
Like other vaccines, evidence shows that rotavirus vaccines are highly effective in preventing severe illnesses that require children to be hospitalized. Reducing hospitalizations from preventable illnesses like rotavirus infection may be especially important for health system capacity at this time, as delivery of many health services in Nigeria has been disrupted by the COVID-19 pandemic7. Introducing rotavirus vaccine in Nigeria offers great potential to reduce the number of hospitalizations in children under five and alleviate pressure on an overburdened health system.
- A 2018 study reported that 46% of children under 5 in Nigeria hospitalized for acute gastroenteritis tested positive for rotavirus8.
- According to a review of 57 articles from 27 countries, hospitalizations due to rotavirus-related acute gastroenteritis (AGE) among children under 5 fell by a median of 67% in the first 10 years after the rotavirus vaccine was licensed9.
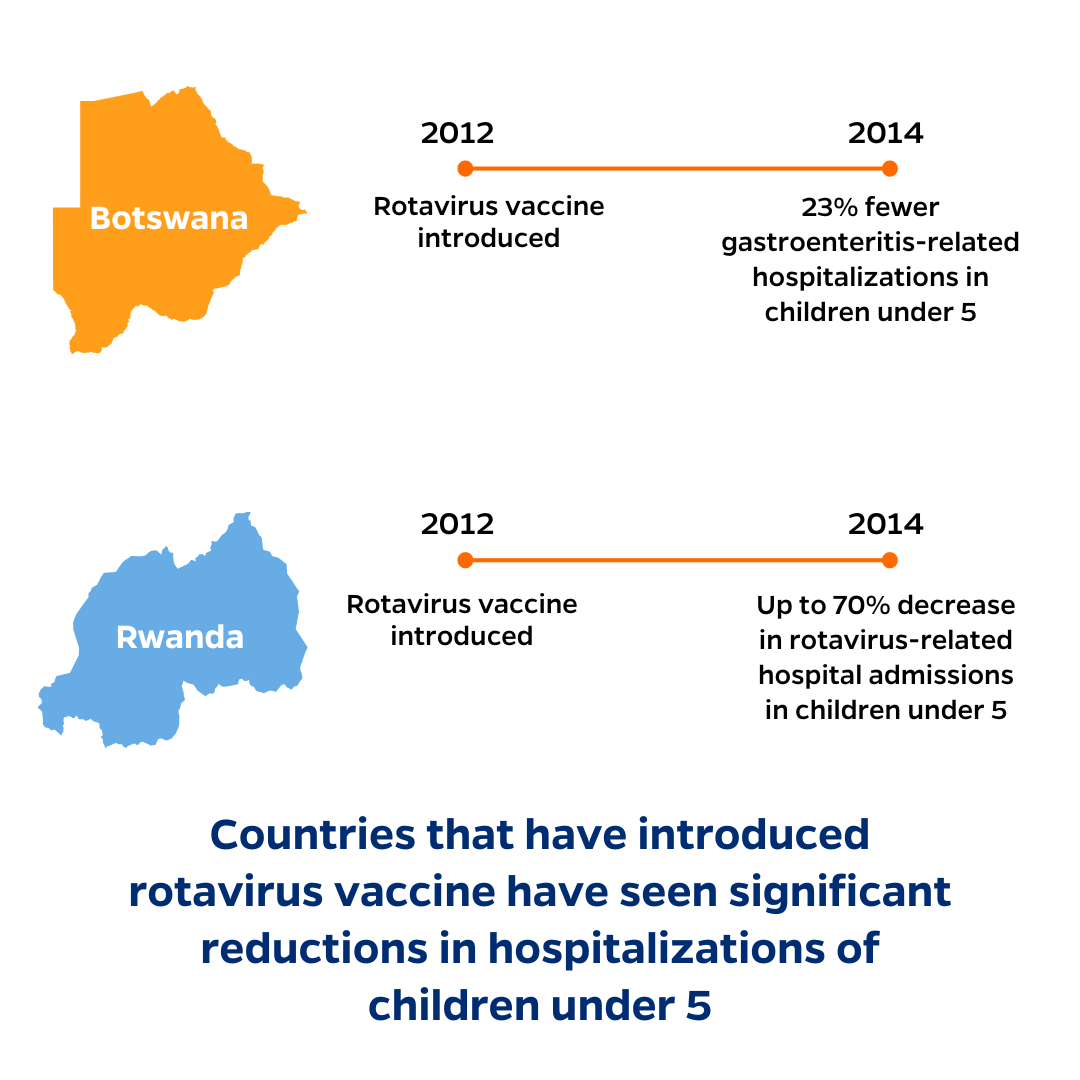
- In Rwanda, hospital admissions due to rotavirus among children under five decreased up to 70% in the two years after the vaccine was introduced10.
- In Botswana, gastroenteritis-related hospitalizations among children under five decreased by 23% in the two years following rotavirus vaccine introduction, with an even larger decline (43%) during the rotavirus season11.
- A review of the vaccine’s impact in the United States found that in the first 11 years of its use, rotavirus hospitalizations declined by an average of 80% among children under five12. Rotavirus-related emergency visits declined by a median rate of 57%.
Rotavirus Vaccine is Cost-Effective & Reduces Financial Burdens on Families
Research shows that like other immunizations, the rotavirus vaccine is cost-effective and provides a positive return on investment for both governments and families.
- In Nigeria, introduction of the rotavirus vaccine is estimated to save the government approximately US$28.5M in healthcare costs over a 10-year period13. These savings translate to a cost per DALY averted of US$116 (95% UI: $69-$169), just five percent of the country’s GDP per capita.
- A meta-regression analysis of the cost-effectiveness of rotavirus vaccination across 195 countries found that it was cost-effective, particularly in LMICs with the highest disease burden14. Among countries eligible for Gavi support, the mean ICER was $255 per DALY averted (95% UI: $39–$918).
- Studies from high-income settings have found that introduction of rotavirus vaccines can provide significant short-term returns on investment (ROI). For example, a series of studies in the United States estimated that once rotavirus vaccines were introduced, the average annual savings in direct healthcare costs from rotavirus and acute gastroenteritis were between US$121M and US$231M12. An economic evaluation of rotavirus vaccination in Italy determined that the cost of introducing the vaccine would be more than offset by savings from prevention of disease cases and hospitalizations within as early as two years15.
Economic Costs of Rotavirus Disease and Value of Vaccines
Families of those treated for diarrheal diseases face significant out-of-pocket expenditures, which can be especially burdensome for those already living in poverty. Many of these costs are considered catastrophic, meaning that they exceed 10 percent of the household’s monthly income. In addition to out-of-pocket medical costs for rotavirus-related illnesses, families who miss work to care for a sick child also face indirect costs due to lost wages. By reducing disease burden, the rotavirus vaccine protects vulnerable families from these catastrophic expenditures.
- In Malaysia, families of those treated for acute gastroenteritis pay an average of US$101 in out-of-pocket costs16. These expenses disproportionately affect families in the lowest income quartile, representing 23% of their monthly household income, compared to less than 6% of monthly household income for families in the highest income quartile.
- The average direct and indirect costs for rotavirus-related diseases among poor families in Bangladesh are US$105.2, including out-of-pocket expenditures for treatment, non-medical costs like transportation and lodging for caregivers, and the opportunity costs of lost wages17. This accounts for nearly one-third of their total monthly household income.
- On average, families in Vietnam lose more than nine working days due to caring for a child with rotavirus18.
Reducing Rotavirus Infections Promotes Healthy Development
Enteric infections like rotavirus can have long-term effects on a child’s development. Diarrheal illnesses often lead to malnutrition, which can cause stunting and impact cognitive development—and which also makes children more susceptible to subsequent infections. Rotavirus vaccine can break this vicious cycle by preventing the malnutrition that accompanies diarrheal diseases to promote healthy growth and development. These vaccines are especially beneficial for children living in low-resource and marginalized communities who are more likely to experience undernutrition and stunting.
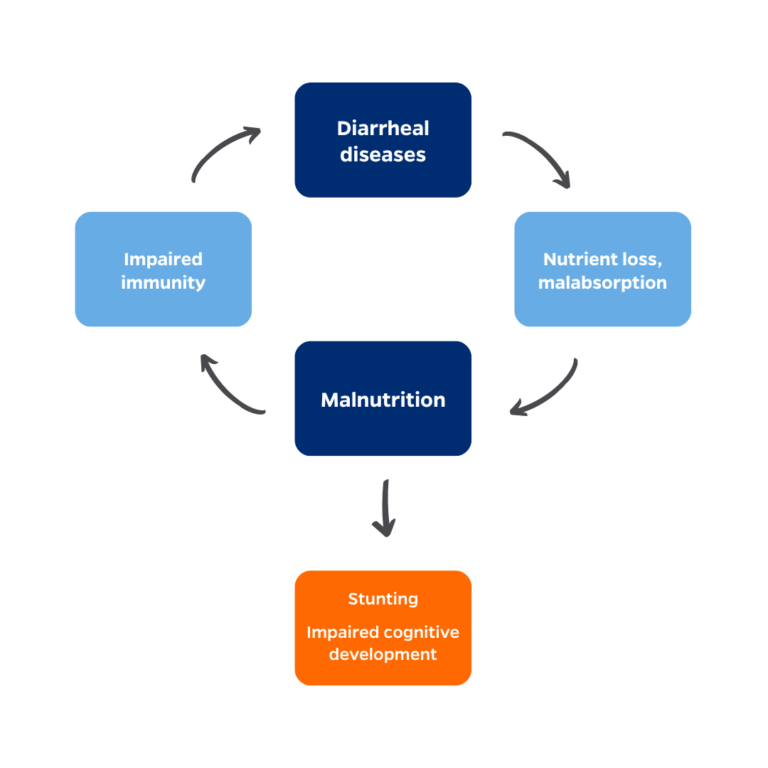
- A pooled analysis of studies from five LMICs demonstrated the cumulative effects of repeat diarrheal episodes from 0–24 months20. For every five episodes of diarrhea that a child experiences, they are 13% more likely to be stunted at age two.
- A study of children in Jamaica found that at age 11 or 12, children who had been stunted by age 2 performed significantly worse than non-stunted children on reading, spelling, and arithmetic tests, even when accounting for socio-economic factors21.
- An analysis of 8,000 children in five LMICs estimated that children who were stunted by age 2 completed an average of approximately one year less of schooling22. They were also 16% more likely than non-stunted peers to have failed a grade.
- Children with diarrhea have a greater risk of developing pneumonia or acute lower respiratory infections (ALRI). A study of children in Ghana estimated that more than 1 in 4 cases of ALRI were attributable to recent diarrheal illnesses, and therefore, preventing diarrheal illnesses would also prevent a large number of pneumonia cases23.
Download This Featured Issue as a PDF
Nigeria’s introduction of rotavirus vaccine is promising, with the potential to protect millions of children from diarrheal diseases caused by rotavirus. Track immunization coverage for rotavirus and other essential vaccines through VIEW-hub, IVAC’s interactive data visualization platform.
References
- International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. (2022). Pneumonia and Diarrhea Progress Report 2022.
- Lanata CF, Fischer-Walker CL, Olascoaga AC, et al. Global causes of diarrheal disease mortality in children <5 years of age: A systematic review. PLoS One. 2013;8(9):e72788. doi:10.1371/journal.pone.0072788
- Tate JE, Burton AH, Boschi-Pinto C, Parashar UD; World Health Organization–Coordinated Global Rotavirus Surveillance Network. Global, Regional, and National Estimates of Rotavirus Mortality in Children <5 Years of Age, 2000-2013. Clin Infect Dis. 2016;62 Suppl 2:S96-S105. doi:10.1093/cid/civ1013
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Institute for Health Metrics and Evaluation (IHME) 2020; Available from: http://ghdx.healthdata.org/ gbd-results-tool.
- International Vaccine Access Center. VIEW- hub. [cited 2022 January]; Available from: http://view-hub.org/.
- Giwa, Omotayo. Nigeria Writes a New Chapter for Child Health with the Introduction of Rotavirus Vaccine. DefeatDD. Published August 22, 2022. Accessed November 17, 2022. https://www.defeatdd.org/blog/nigeria-writes-new-chapter-child-health-introduction-rotavirus-vaccine
- Shapira G, Ahmed T, Drouard SHP, et al. Disruptions in maternal and child health service utilization during COVID-19: analysis from eight sub-Saharan African countries. Health Policy Plan. 2021;36(7):1140-1151. doi:10.1093/heapol/czab064
- Tagbo BN, Mwenda JM, Eke CB, et al. Rotavirus diarrhoea hospitalizations among children under 5 years of age in Nigeria, 2011-2016. Vaccine. 2018;36(51):7759-7764. doi:10.1016/j.vaccine.2018.03.084
- Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD. Global Impact of Rotavirus Vaccination on Childhood Hospitalizations and Mortality From Diarrhea. J Infect Dis. 2017;215(11):1666-1672. doi:10.1093/infdis/jix186
- Ngabo, F., Tate, J.E., Gatera, M., et al 2016. Effect of pentavalent rotavirus vaccine introduction on hospital admissions for diarrhea and rotavirus in children in Rwanda: a time-series analysis. Lancet Global Health. 4:e129-36.
- Enane LA, Gastanaduy PA, Goldfarb DM, et al. 2016. Impact of rotavirus vaccination on hospitalizations and deaths from childhood gastroenteritis in Botswana. Clinical Infectious Diseases. 2016(2).
- Pindyck T, Tate JE, Parashar UD 2018. A decade of experience with rotavirus vaccination in the United States – vaccine uptake, effectiveness, and impact. Expert Review of Vaccines. 17(7).
- Debellut, F., Clark, A., Pecenka, C., Tate, J., Baral, R., Sanderson, C., … & Atherly, D. 2019. Re-evaluating the potential impact and cost-effectiveness of rotavirus vaccination in 73 Gavi countries: a modelling study. The Lancet Global Health. 7(12).
- Janko MM, Joffe J, Michael D, et al. Cost-effectiveness of rotavirus vaccination in children under five years of age in 195 countries: A meta-regression analysis. Vaccine. 2022;40(28):3903-3917. doi:10.1016/j.vaccine.2022.05.042
- Carroll S, Rojas AJ, Glenngård AH, Marin C. Vaccination: short- to long-term benefits from investment. J Mark Access Health Policy. 2015;3:10.3402/jmahp.v3.27279. Published 2015 Aug 12. doi:10.3402/jmahp.v3.27279
- Loganathan, T., Lee, W.S., Lee, K.F., et al 2015. Household Catastrophic Healthcare Expenditure and Impoverishment Due to Rotavirus Gastroenteritis Requiring Hospitalization in Malaysia. PLOS One. 10(5).
- Ahmed S, Dorin F, Satter SM, et al. The economic burden of rotavirus hospitalization among children < 5 years of age in selected hospitals in Bangladesh. Vaccine. 2021;39(48):7082-7090. doi:10.1016/j.vaccine.2021.10.003
- Riewpaiboon A, Shin S, Le TP, et al. Cost of rotavirus diarrhea for programmatic evaluation of vaccination in Vietnam. BMC Public Health. 2016;16(1):777. Published 2016 Aug 11. doi:10.1186/s12889-016-3458-2
- Guerrant RL, DeBoer MD, Moore SR, Scharf RJ, Lima AA. The impoverished gut–a triple burden of diarrhoea, stunting and chronic disease. Nat Rev Gastroenterol Hepatol. 2013;10(4):220-229. doi:10.1038/nrgastro.2012.239
- Checkley, W., Buckley, G., Gilman, R.H., et al. 2008. Multi-country analysis of the effects of diarrhoea on childhood stunting. International Journal of Epidemiology. 37(4).
- Chang SM, Walker SP, Grantham-McGregor S, Powell CA. Early childhood stunting and later behaviour and school achievement. J Child Psychol Psychiatry. 2002;43(6):775-783. doi:10.1111/1469-7610.00088
- Martorell R, Horta BL, Adair LS, et al. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analyses from five birth cohorts from low- and middle-income countries. J Nutr. 2010;140(2):348-354. doi:10.3945/jn.109.112300
- Schmidt WP, Cairncross S, Barreto ML, Clasen T, Genser B. Recent diarrhoeal illness and risk of lower respiratory infections in children under the age of 5 years. Int J Epidemiol. 2009;38(3):766-772. doi:10.1093/ije/dyp159
Resource Type:
Report
Practice Areas:
Technical Advocacy
Location:
Nigeria
Target Population:
Child